What is Frozen shoulder ?

Adhesive capsulitis, another name for frozen shoulder, is a painful condition where the shoulder’s range of motion is restricted.
The shoulder joint capsule—a thick, stiff, and inflammatory band of connective tissue around the shoulder joint—becomes frozen shoulder when this happens. (The ligaments that firmly secure the joint in place by joining the top of the upper arm bone (humeral head) to the shoulder socket (glenoid) are located within the joint capsule. The “ball and socket” joint is a more familiar name for this joint.)
Because the shoulder is less likely to be used the more painful it is, the condition is known as “frozen shoulder.”
When the shoulder isn’t used, the capsule thickens and tightens, making it increasingly harder to move because the shoulder is “locked” in place.
Who is susceptible to frozen shoulder?
Adults, typically between the ages of 40 and 60.
More prevalent in women than in men.
Recent shoulder injury: Any operation or damage to the shoulder that necessitates immobilization (i.e., by using a shoulder brace, sling, shoulder wrap, etc.). A rotator cuff tear and fractures of the shoulder blade, collarbone, or upper arm are two examples.
Frozen shoulder affects between 10 and 20 percent of those with diabetes mellitus.
Stroke, hypothyroidism (an underactive thyroid gland), hyperthyroidism (an overactive thyroid gland), Parkinson’s disease, and heart disease are among the other illnesses and ailments. Because a stroke may impede arm and shoulder movement, it is a risk factor for frozen shoulder. It is unclear why various illnesses and disorders raise the possibility of having a frozen shoulder.
Causes and Symptoms
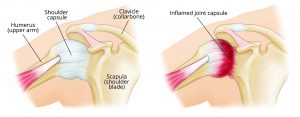
In frozen shoulder, the smooth tissues of the shoulder capsule become thick, stiff, and inflamed.
The four stages of frozen shoulder development are usual. Physiotherapy treatment can accelerate its remission and help you regain function.
First Stage: “Pre-Freezing”
If adhesive capsulitis has been identified as the cause of your symptoms, you have undoubtedly been dealing with it for some time. The shoulder hurts day and night, getting worse when you try to move it, although it might hurt even when it is not being utilized. You’ll notice that your range of motion has slightly diminished, and you’ve used your shoulder less because of the discomfort.
Movement loss is more obvious when you raise your arms or reach behind your back, while pain is most visible when you extend one arm away from your body.
Second stage: “Freezing”
The freezing stage often occurs after three to nine months of symptoms; nighttime discomfort will have gotten worse along with a growing loss of shoulder motion; and range of motion is still restricted by pain and stiffness.
Third stage: “Frozen”
Symptoms have been present for nine to fourteen months at this point, and range of motion has been significantly diminished. Early on in this stage, there is a significant degree of agony, which lessens as the frozen period comes to a close. The shoulder may then only experience pain when it is moved to its maximum range of motion.
Fourth stage: “Thawing”
Typically, after twelve to fifteen months of symptoms, the discomfort has subsided, especially at night. Although the range of motion is still restricted, it is slowly improving.
The diagnosis of frozen shoulder
In order to identify frozen shoulder, your doctor will suggest some tips and methods:
Doctors recommend to discuss your symptoms and review your medical history in INIGIMA Cloud Diagnosis.
Examine your arms and shoulders physically. The doctor will move your shoulder in all directions to determine its range of motion and whether it hurts when you move it. Finding your “passive range of motion” involves an examination in which your doctor moves your arm rather than you.
In order to determine your “active range of motion,” the doctor will also watch you move your shoulder.
The two motions are contrasted. The range of motion for those who have frozen shoulders is constrained, both actively and passively.
In order to confirm that another shoulder issue, like arthritis, is not the source of the symptoms, normal shoulder X-rays are also taken. In most cases, frozen shoulder can be diagnosed without the use of sophisticated imaging techniques like ultrasonography and magnetic resonance imaging (MRI). They might be examined to rule out other issues, like a torn rotator cuff.
Messages at home can reduce the pain
- Insidious shoulder stiffness and a nearly complete loss of passive and active external rotation are common symptoms of frozen shoulder.
- The three stages of frozen shoulder—freezing (painful), frozen (sticky), and thawing—occur sequentially and are frequently self-limiting.
- NSAIDs, intra-articular injections of glucocorticoids, and/or physical therapy are typical conservative therapies for frozen shoulder.
- First-line treatments for frozen shoulder may include physical therapy and at-home exercises, depending on the patient’s symptoms and the severity of the condition.
- Gentle stretching exercises can be performed during the freezing (painful) period, but they should be confined to a brief duration (1–5 seconds) and not exceed the patient’s pain threshold.
- Strengthening activities such scapular retraction, posterior capsule stretch, and isometric shoulder external rotation can be introduced to the patient’s routine during the frozen (adhesive) period to maintain muscle strength.
- The patient gradually regains range of motion throughout the thawing period. Stretching and strengthening exercises can be intensified, with longer holding times.
Key Points :
INIGIMA Digital Screening plays a very important role if you are suffering from multiple complications like diabetes, blood pressure, heart issues and obesity patient. It helps to maintain good health and helps to achieve a longer life. Book a session with an expert now
A review article by
(Clinical Research Director @ IEEARC Tech)
Comments are closed