Evaluating the Clinical Utility of Hematological Ratios in Sickle Cell Anemia
Manisha Shukla 1, Rohit Kumar Vishwakarma 1, Anjali Tomar 2
Vol 1/Issue 3
Abstract
Sickle Cell Disease (SCD) is a genetic blood disorder that affects the shape and characteristics of red blood cells. It can manifest a range of symptoms characterised by chronic hemolytic anaemia, recurrent infections, acute pain crises, and organ damage that vary in severity and frequency among individuals. In Indian tribal populations, it is a significant contributor to obstetric problems and pregnancy risk. Neutrophil to Lymphocyte Ratio (NLR), Platelet to Neutrophil Ratio (PNR) and Platelet to Lymphocyte Ratio (PLR) are the three important biomarkers derived from blood tests that can provide insights into the clinical severity of SCD patients. This study understands the potential clinical utility to determine NLR, PNR and PLR in SCD patients.
Three hematological ratios were calculated for each patient: NLR, PLR, and PNR. NLR was derived by dividing the absolute neutrophil count by the absolute lymphocyte count. Similarly, PLR was obtained by dividing the platelet count by the absolute lymphocyte count, and PNR was calculated as the ratio of the platelet count to the absolute neutrophil count.
The NLR and PLR ratios was found significantly higher in patients than controls, suggesting that enhanced NLR is linked to anaemia. While, PNR ratio was found significantly lower in patients than controls. The NLR, PNR and PLR values may be useful as prognostic markers in SCD patients. Although the genetic and molecular underpinnings have long been identified, the pathophysiology is still poorly understood. Therefore, using pathophysiological data to detect SCD severity early may be helpful in managing sickle cell anaemia patients.
Introduction
Millions of people worldwide are impacted by Sickle Cell Disease (SCD), which has a significant healthcare cost. SCD is a genetic blood disorder caused by a mutation in the hemoglobin gene, leading to the production of abnormal haemoglobin, known as hemoglobin S (HbS). It primarily affects red blood cells, causing them to become rigid and misshapen. Unlike normal, flexible red blood cells, the sickle-shaped cells are rigid and sticky, which hampers their ability to flow smoothly through blood vessels. The irregular shape of these cells causes them to clump together, blocking small blood vessels and interrupting normal blood flow. Such interruptions lead to severe complications, including pain, anemia, and organ damage, significantly impacting the quality of life for affected individuals (1). Identifying early biomarkers of disease severity is critical for effective disease management (2, 3). The study aims to investigate the potential clinical utility of hematological indices: Neutrophil-to-Lymphocyte Ratio (NLR), Platelet-to-Lymphocyte Ratio (PLR), and Platelet-to-Neutrophil Ratio (PNR) as markers of disease severity in SCD patients.
Materials and Methods
The study utilized patient records sourced from a District Hospital Shahdol, Madhya Pradesh, covering the period from 2022 to 2024. These records included demographic data and laboratory results. The target population above 5 years old, both male and female, diagnosed with Sickle Cell Anemia. Data filtering was performed to exclude incomplete or inconsistent records, ensuring the accuracy and reliability of the analysis.
Hematological Indices Calculation
NLR: Neutrophil Count/Lymphocyte Count PLR: Platelet Count/Lymphocyte Count PNR: Platelet Count/Neutrophil Count
Statistical analysis performed between SCA patients (n=100) and controls (HbAA, n=100). Comparative analysis was performed to explore variations in NLR, PLR, and PNR across subgroups, such as age, gender, and disease severity. Ethical approval was secured, and patient
confidentiality was upheld. The findings aimed to evaluate the clinical utility of NLR, PLR, and PNR as potential biomarkers for monitoring and prognosis in SCD.
Result
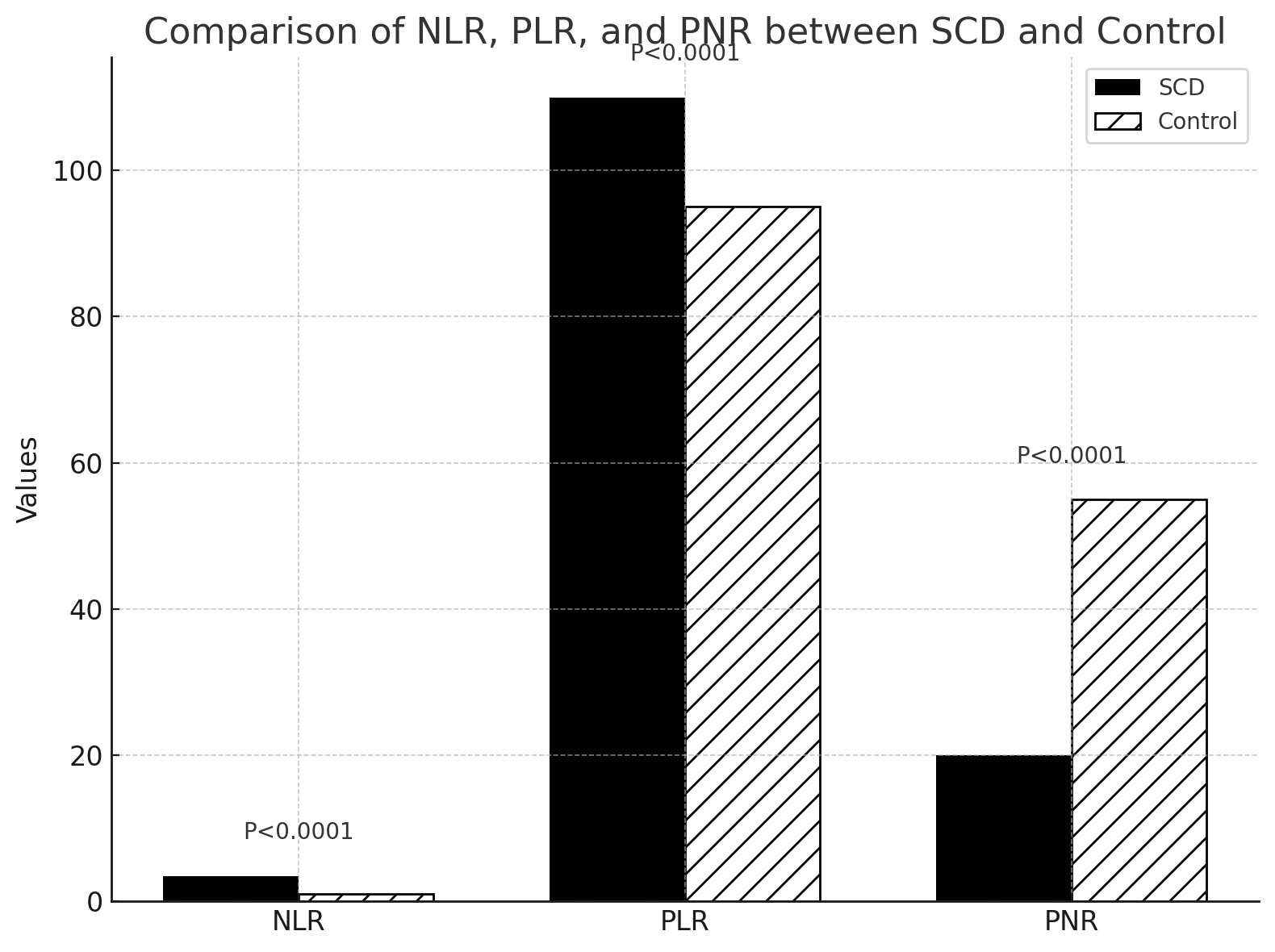
The study highlights significant differences in hematological indices between SCD patients and the control group (Figure 1 and Table 1 , indicating their potential utility as biomarkers for disease severity:
| Parameter | SCD Group | Control Group | P-value |
|---|---|---|---|
| NLR | ~3.5 | ~1.0 | <0.0001 |
| PLR | ~110 | ~95 | <0.0001 |
| PNR | ~20 | ~55 | <0.0001 |
Table : 1
- NLR: The average NLR was significantly higher in SCD patients (1.31 ± 0.02) compared to the control group (1.18 ± 0.03), with a p-value of less than 0.0001, suggesting heightened inflammatory activity in SCD.
- PLR: Similarly, PLR was markedly elevated in SCD patients (102.7 ± 3.1) versus controls (91.2 ± 2.4), with a p-value of less than 0.0001, reflecting altered platelet activity in the disease state.
- PNR: In contrast, PNR was significantly reduced in SCD patients (13.9 ± 2.67) compared to the control group (56.15 ± 4.43), also with a p-value of less than 0.0001, pointing to dysregulation in platelet and neutrophil interaction.
These differences underline the role of NLR, PLR, and PNR as promising markers to assess disease severity and progression in SCD.
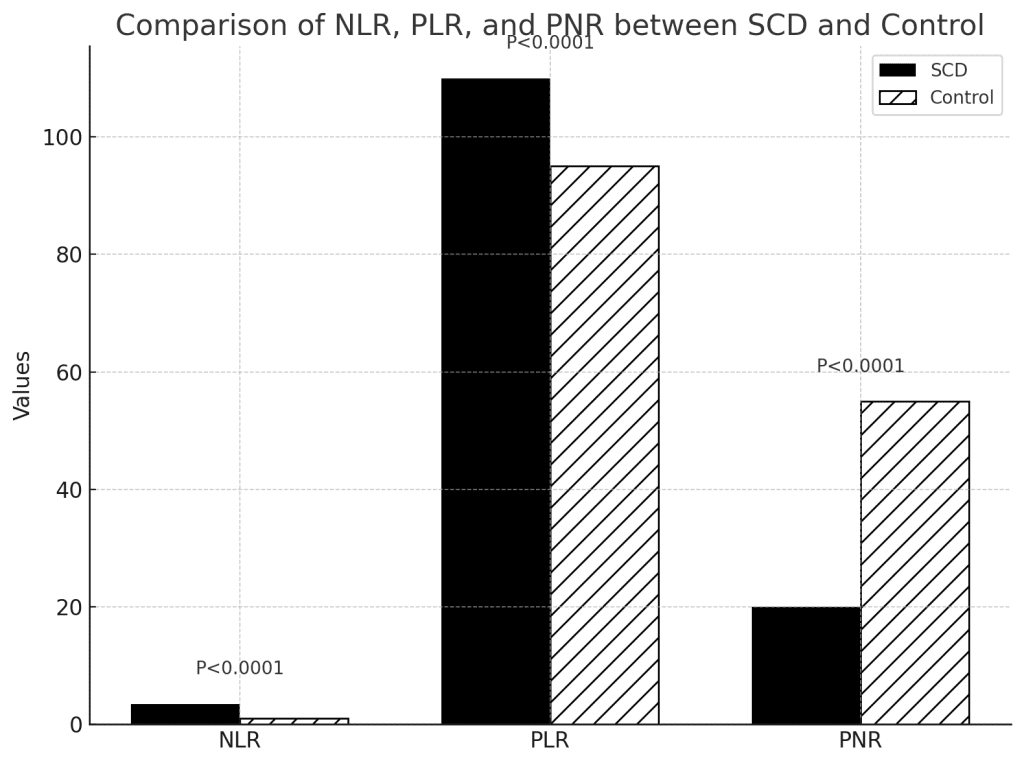
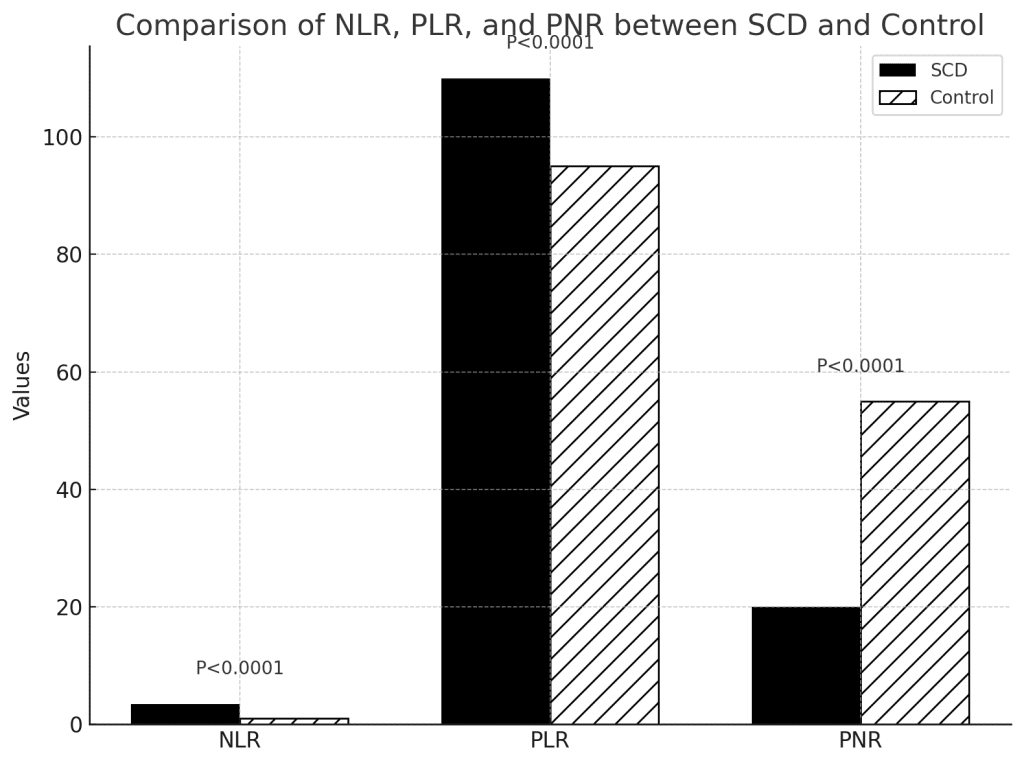
Figure1: Comparison of NLR, PLR and PNR
Discussion
The elevated NLR and PLR in SCD patients indicate heightened inflammatory activity, reflecting disease severity (4). Reduced PNR suggests dysregulated platelet function and neutrophil activity, possibly exacerbating vascular complications. The significant differences in these indices between SCD patients and controls highlight their diagnostic and prognostic potential (5).
Conclusion
This study underscores the clinical relevance of NLR, PLR, and PNR as biomarkers for disease severity in Sickle Cell Anemia. These indices offer a non-invasive and cost-effective approach for monitoring disease progression and tailoring treatment, ultimately improving patient outcomes and quality of life. Further studies are needed to validate these findings and explore their utility in guiding personalized treatment strategies.
Acknowledgement
This work was supported by Pandit S.N. Shukla University Shahdol, District Hospital Shahdol, MANIT Bhopal M.P., Govt. Medical College Shahdol M.P and IEEARC Technologies Pvt Ltd New Delhi and Its Investment Partners / Incubation IIM-A, Delhi Govt.
AUTHOR INFORMATION
Corresponding Author
Manisha Shukla − Department of Biotechnology, Pandit S.N. Shukla University, Shahdol, Madhya Pradesh, India 484001
Email: mshukla@bt.iitr.ac.in
Phone: +91- 8839096157
Authors
Rohit Kumar Vishwakarma
Department of Biotechnology, Pandit S.N. Shukla University, Shahdol, Madhya Pradesh, India 484001
Anjali Tomar
Department of Biotechnology, Pandit S.N. Shukla University, Shahdol, Madhya Pradesh, India 484001
References
- Kumari R, and Shukla M. 2023. Sickle Cell Anaemia: Case Presentations from the Indian Tribal Population and Discussion on the Clinicopathologic Aspects.Int.J.Curr.Microbiol.App.Sci. 12(9): 67-79.
- Emokpae MA, Abdu A, Gwaram B A. Neutrophil-to-lymphocyte, platelet-to-lymphocyte ratios and their association with atherogenic index of plasma in sickle cell nephropathy. J Appl Hematol 2016;7:24-9.
- Efobi CC, Nri-Ezedi CA, Madu CS, Ikediashi CC, Ejiofor O, Ofiaeli CI. Neutrophil- Lymphocyte, Platelet-Neutrophil, and Platelet-Lymphocyte Ratios as Indicators of Sickle Cell Anaemia Severity. Ethiop J Health Sci. 2023 Sep;33(5):821-830.
- Chukwurah E, Obeagu E, Emodi N. Leucocyte count in children with sickle cell anaemia comparative values in steady state, vaso-occlusive crisis state and bacterial infection. Ejpmr. 2019;6:706–714.
- Aneke J, Adegbola O, Emmanuel C, Christian E, Nancy C, Muheez A. Neutrophil to Lymphocyte Ratio in Sickle Cell Anaemia Patients with Nephropathy. Br. J. Med. Med. Res. 2015;10:1–6. DOI: 10.9734/bjmmr/2015/20404.